*Poznan University of Medical Sciences
https://orcid.org/0000-0003-2833-8815
email: justynaczekajewska@gmail.com
**Nicolaus Copernicus University in Toruń
https://orcid.org/0000-0003-2470-8823
email: zimnya@umk.pl
According to the International Register of Organ Donation and Transplantation, Japan is one of the countries with the lowest number of registered deceased donors. In 2019, Japan was ranked 61st out of 70 countries. The authors of this article have decided to explore the reasons for this phenomenon. In the first part of the work, religious influences (Shinto and Buddhism), the tradition of gotai manzoku, the importance of altruism and the family in the perception of death and organ transplantation by the Japanese are considered. The second part of the article presents the arguments of Alan Shewmon, who believes that brain death is not death in the biological sense. Undermining the brain’s death criterion raises doubts concerning death of patients in irreversible coma, what in result discourages transplantology in Japan. In the third part, the authors compare the results of JOTN, IRODaT and the Fact Book of Organ Transplantation 2018 in Japan from 2010 to 2018. The aim of the article is to explain the cultural determinants of transplantology in Japan, taking into account the influence of philosophical and bioethical aspects of human death.
Keywords: transplantation, brain death, Japan, JOTN, philosophical monism, Shinto, gotai manzoku tradition.
The first human organ transplant was carried out in 1954 and after that the issue of the precise definition of death became more than a philosophical question. It is a foundation that enables ethical organ procurement, and consequently, a successful life-saving procedure for a great number of patients. Moreover, the perception of brain and cardiac death goes beyond scientific analysis and arguments – it is the cultural and religious background that in many cases shapes citizens’ views on organ donation, as well as the stance on brain death itself.[1]
Japan belongs to the group of developed countries with the lowest numbers of deceased transplant donors.[2] This situation is largely attributed to Japanese culture and to the great role played by traditional values in Japanese society. Moreover, unsuccessful attempts in the early history of Japanese transplantation contributed to the unfavourable public perception of the practice. The first transplant from a brain-dead donor in Japan, remembered today as the ‘Wada Incident’, took place in 1968. Professor Jurō Wada of Sapporo Medical College attempted a heart transplant, but the recipient died, and soon questions were raised concerning both the choice of the recipient and the brain death diagnosis of the donor. As a result, Wada was charged with a double murder and the Japanese government placed a moratorium on transplants from brain-dead donors.[3] It lasted until 1997, when the Organ Transplant Law allowed organ procurement from brain-dead donors who had left written consent. The law was further revised in 2009, allowing procurement with family consent, including minor donors (younger than fifteen). These legal changes, however, did not lead to a major increase in the number of transplants.
Today, making a donor declaration in Japan is simple: a Japanese health insurance card, compulsory for all residents, also serves as a donor card, and allows its holders to state if they agree to organ procurement and if there are any specific organs that they wish to withhold. People can also opt for one of two definitions of death: circulatory or brain death. Even so, the lack of widespread and systematic information leaves a number of residents unaware or uninterested in these options, particularly the older generations (people in their 60s and 70s).[4]
This article explores the reasons behind the limited interest in organ donation in contemporary Japan, focusing on the data from 2010 to 2018. The first part discusses the cultural background: religious influences and their limitations related to secularization, popular folk beliefs, traditional interpersonal obligations framed within the context of altruism and finally how the media coverage of the issue shapes the general public’s perception on organ donation. Part two presents changes in the definition of death resulting from the development of medical science. It addresses the arguments of Alan Shewmon that shift the focus from organ procurement from brain-dead donors to the methods of monitoring brain activity. Many Japanese researchers share his attitude and focus on helping patients in comas rather than pursuing organ donation from people diagnosed with brain death. The transplant-related numbers introduced in part three present changes in the organ donation arena after the legal reform of 2009. Finally, the fourth part discusses governmental policies to be introduced with the purpose of increasing interest in organ donation, including general system and facilities improvements and ethics education for the youngest citizens. These proposals not only introduce ways of future improvements, but also shed light on the current system’s weaknesses that may have had an influence on the limited interest of Japanese citizens in organ donations.
The article offers a multifaceted analysis of the factors that hinder the number of organ transplants in contemporary Japan, particularly the debates surrounding the definition of death and the superior role of the brain in the human body.
There are a number of reasons why the idea of organ transplantation has not yet been fully accepted by the Japanese society. Religious influences, the culture of social interaction, traditional family roles and finally the influence of medicine, can be listed among them.
Articles shedding light on the low numbers of organ donations often link the situation to religious background.[5] The main religions of Japan are Shinto and Buddhism. The Japanese, however, often tend to practice different religions depending on the occasion instead of dedicating themselves strictly to one system of beliefs. In this approach, Buddhism is mainly related to the issues of death and funeral rites, as of today about 90% of funeral ceremonies are Buddhist.[6] It is, therefore, Buddhism that primarily influences beliefs concerning death, and consequently, deceased-donor organ transplants.
Japanese Buddhism does not have a single unified doctrine but is rather divided into several schools expressing complex opinions towards deceased-donors transplants in general, as well as the notion of brain death specifically. The practice of transplantation itself is not perceived as wrong, and is even recognised by some as a fuse, a Buddhist selfless offering linked to the virtue of generosity. Nevertheless, Honganji, the largest school of Jōdo Shinshū (Shin Buddhism), the branch of Buddhism with the largest number of adherents in Japan, took an official negative stand on the amendments made in the Organ Transplant Law in 2009 that allowed the family to decide on the organ donation issue, even if the deceased had not left a will on that matter. In an open letter to the President of the House of Councillors, Eda Satsuki, Honganji Gov. General Kōshō Fujikawa criticized organ procurement from minors as well as the possibility of the family making a decision against the deceased’s will.[7] Furthermore, he urged that priority be given to saving the life of a potential donor and conducting extensive research on the definition of brain death. Another school, Tendai, also recognizes deceased-donor transplants as not being in contradiction to Buddhist teachings. It can be executed, however, only under the condition that there is no chance to cure a donor who had left a written statement concerning donation, and that the recipient takes part in a religious rite to celebrate the dignity of life.[8]
While the largest schools educate their followers on the established limitations of organ transplant based on their doctrine, individual scholars still seek a definitive interpretation of Buddhist teachings in that matter, and they frequently reach contradictory conclusions. Tetsuo Yamaori, a religious studies scholar who opposes transplants, has raised arguments related to the proper and worthy way of meeting death and to humanity’s equal place among other living creatures that should result in simply accepting death as natural element of life rather than going to extremes to save human beings.[9] His views were criticized by Yoshitsugu Watanabe, an ethics researcher who accused Yamaori of generalizations only based on selected parts of Buddhist teachings, without the proper context being taken into account.[10] Buddhist scholars are therefore not unanimous about the issue, and their opinions remain dissenting, without any major influence on the present doctrine.
On the other hand, the indigenous, animistic, pantheistic Japanese religion of Shinto, lacks a fixed doctrine and organisation, and consequently does not take an official stance on transplants. A few voices from Shinto scholars and clergy, however, dissuade believers from accepting the idea of brain death. Masahiro Izawa, a Shinto scholar, emphasizes the ultimate sanctity of life, gifted to one through generations of ancestors. One person cannot be deprived of life to save another, and the body should be treated with the utmost respect even after death.[11] Potential organ procurement may only take place after a patient’s life support system has been turned off and after their subsequent circulatory death. Similar concerns were voiced by the Shinto priest Takahiro Nakajima, who added that while self-sacrifice is morally acceptable in extreme cases, it should not be normalized and turned into everyday practice in the form of brain-dead donations.[12] Some Western literature links the lack of acceptance for transplants in the case of Shinto with the concept of impurity, kegare.[13] Ritual uncleanness in Shinto results from any contact with death, disease, menstruation, or childbirth, and requires purification. Despite the Western assumption that a fear of kegare may influence transplant decisions, Japanese-language sources do not link these two issues.
The main Buddhist schools tentatively approve of the general idea of dead-donor transplants under specific circumstances, while Shinto lacks a unified, official stance on the issue. The Japanese Association of Religious Organizations,[14] which supports cooperation between Japan’s main religious denominations, issued a joint statement in 2009 criticizing the Organ Transplant Law Revision of the same year. However, this criticism did not extend to transplants from brain-dead patients if the decision was made consciously by the donor before death. Moreover, there are no religious issues with donations after circulatory death or from living donor transplants.[15] Simultaneously, much of the inconclusive doctrinal debate surrounding the potential religious wrongness of transplants remains in academic circles, with a limited impact on the general public. Given the progressing rate of secularization of Japan and the concomitant decline of the impact of religious teachings, doctrines should not be considered the most decisive factor influencing the number of transplants.[16]
An additional element that should be considered among religious doctrines are the teachings of Confucius, since they are still relevant for the culture and society of modern Japan. Confucianism in contemporary Japan is not a religion like Buddhism and Shintoism: there are no doctrines, clergy or schools that would voice opinions on ethical issues. Nevertheless, although ”almost no one considers himself a Confucianist today, (...) in a sense almost all Japanese are.”[17] Confucian ethical values are at the heart of Japanese views on harmony, loyalty, the value of education, and hard work.[18] Confucianism is considered one of the factors hindering organ donation in East Asia, since it emphasizes the virtue of xiao, filial piety, which means respect for parents and ancestors. Consequently, an ”individual has an essential ethical obligation to ensure that at death his or her body is returned intact to their ancestors.”[19] Furthermore, ”one must safeguard what one has received from parents and must not disregard them”[20] and since the body was received from one’s parents, it cannot be damaged. Some scholars have argued, however, that organ donation is in the spirit of the Confucian virtue of ren, humanity or benevolence[21], so properly interpreted Confucian teachings should not be perceived as discouraging to potential donors. Nevertheless, in contemporary Japan, not many Japanese are familiar with the classical Confucian teachings. A potential influence of Confucianism on organ donation lies therefore in its impact on traditional family structure (its role in limiting transplants is discussed in 2.4) rather than in interpretation of the teachings itself.
More so than religion, it is the general Japanese worldview and the beliefs more or less loosely rooted in traditional religions that should be taken into account. Such “folk religion”, understood as the “aggregate of beliefs and practices arising from both orally transmitted indigenous religious beliefs and customs, and Japanese popular religion (the forms taken by lay observance of literate established religions)”[22] shapes to a certain extent the Japanese perception of death and the dead body.
As Buddhism and Shinto were deeply interlinked for centuries, so called Shinbutsu-shūgō (syncretism of kami, meaning Shinto deities, and buddhas) emerged. As a result, some of its beliefs are rooted in both religions, like the deification of the ancestors’ souls for example. According to Shinto, spirits of the deceased become kami, deities, and keep watching over their descendants. This belief is the foundation of ancestral worship.[23] Interestingly enough, one of the numerous terms to describe a deceased person or their soul is hotoke. The word carries multiple meanings such as an ”enlightened person”, as well as even referring to Gautama Buddha himself. Traditionally, the beliefs of the Japanese folk did not separately define kami, hotoke and ancestors and let all three of them intertwine closely, reinforcing the concept of apotheosis of the dead.[24] The sacred element in the perception of the deceased can be seen as one of the factors hindering the increase in organ donations, as the perspective of “depriving” a deity of a body part could raise concerns.
Another belief deeply rooted in Japanese society is “the wholeness of the body”. Gotai manzoku, meaning “perfection of five body parts”, presents a concept of leaving the whole body – head and four limbs – intact. This concept is also sometimes argued to be the reason why tattooing and piercing are not widespread practices in Japan, as they violate the integrity of the body. Moreover, if the body after death is not buried or complete, the soul of the deceased cannot rest in peace[25] and this notion can also lead to some doubts concerning organ donations. Even a cremated body, as long as all ashes remain together, is believed to be gotai manzoku. The wish to fulfil this requirement can lead to some doubts concerning organ donations: whatever happens to the body, happens also to the ancestor’s soul in the afterlife, so “hurting” the body in any way means “hurting” the deceased family member who should be respected and protected.[26] This argument concerning gotai manzoku seems to be more important to family members who make final decisions about organ donation, especially when it comes to the older generations, than to potential donors themselves. While academic discussion on the relevance of this concept to Japanese transplantology is still limited, the idea is present in media coverage on personal accounts and debates regarding organ donation.[27]
It is not only the body parts that are inseparable: in the traditional Japanese worldview, contrary to Christian culture, body and soul are an integrated whole, something that developed and grew as one perfect construct. Translated into English, the term kokoro means heart (organ), spirit/soul and mind, as they can be perceived as one entity and therefore they are named with the same word. By extension, human beings are an integral part of the divine world of nature:
Nature is traditionally interpreted as a superior and mysterious force of either a creative or destructive character, which resides in natural elements, animals, and certain human beings (...). Thus, human beings are not considered to be superior or opposed to nature, as they are in western thought; their lives are embedded in it. This concept of nature leads to the doctrine that everything that is born must die and that nothing remains unchanged.[28]
Hence, organ procurement can be seen as going against nature, an infringement upon the wholeness that characterises and links all living creatures.
This traditional worldview rooted in folk belief can, therefore, cause certain reluctance towards organ transplants among the Japanese. There are, however, further factors influencing donation numbers related to the culture of social interactions and structure.
Several scholars have mentioned the Japanese concept of altruism as a deterrent to donations.[29] Altruism in Western culture, the selfless act of giving something just to benefit society while expecting no reward for it, is often quoted as one of the important motivations for organ donations.[30] In Japan, however, the weight is placed on the reciprocal altruism, and its role in founding identifiable, interpersonal relationships. The term giri, social obligations, means a practice of returning benevolence. Today, it often takes the form of a customary gift exchange which ensures social harmony. One’s social obligations change in accordance with the other person’s position in the uchi/soto circle. Uchi means ”inside, home”, whereas the meaning of soto is “outside, others.” Family, relatives and people with whom a close relationship was established belong to uchi, and it is one’s responsibility to take care of them. There is, however, no expectation of altruism directed towards soto people. Consequently, since the donor cannot expect anything in return, “the idea of giving objects of value to complete strangers with whom one has had no personal contact appears strange to many.”[31] Moreover, Lock’s research suggests that a significant number of potential donors would authorize organ procurement if they could establish a relationship with the recipient first.[32]
Traditionally, the life of a Japanese is firmly located within a net of interpersonal relationships in which harmony, loyalty and respect for the elders play crucial roles. As life is shaped by relationships, with the main focus on family, so is death. Illness and death are family matters, not up to an individual to decide. Although informed consent is a broadly accepted practice in Japan, in the cases of terminal diseases, physicians often inform the family first, and only after receiving their consent they proceed to share information with the patient.[33] Furthermore, even if the patient signed the donor card, it is up to the family to make the final decisions about donations.
A 2013 Cabinet Office poll targeting approximately 3000 Japanese citizens suggests that the same people who were willing to become donors themselves, remained reluctant when asked about giving consent concerning a family member and they listed fear of regret in the future, inability to make proper judgment and the generational gap as some of the reasons.[34] Strong family bonds are still a cultural fundament of Japanese society. Despite the fact that, pursuant to the current legislation, a family can issue consent to donate body organs of the deceased who did not sign a donor card, such decisions may remain rare in the near future.
Another strongly family-oriented country struggling with an extreme shortage of organ donations is China, where social order has also been built on Confucian teachings. Fan and Wang have noted that the misunderstood virtue of filial piety causes adult children to be reluctant to fulfil their parents’ wishes to donate organs. Similarly to the Japanese, they are concerned that funeral rituals might be disrupted by organ procurement and they are also afraid of being disrespectful.[35] On the other hand, Spain, with its family-oriented society, is a country with the highest organ donation ratio in the world.[36] Strong family bonds are not unique to Japanese society and therefore should not be perceived as a factor necessarily limiting organ donations. Other social and cultural factors, like the influence of Confucianism on family values, should be take into consideration.
Further deterrents, partially interlinked, result from the unfortunate history of Japanese transplants from brain dead donors. The 1968 Wada incident generated considerable distrust against medical institutions in Japanese society and the notion of brain death, as well as concerns regarding safety of a potential donor, such as the priority to diagnose brain death to enable transplant over providing the potential donor with every possible life-saving medical care. A clinical professor, Motohide Shimazu, pointed out in a press interview that, currently, brain death diagnosis is usually given by an emergency physician, or by a neurologist if the hospital can provide one, and a transplant surgeon is not even consulted.[37]
In information broadly available to Japanese citizens, the criteria for brain death remain unclear. Campaigns to promote transplant awareness, like the country-wide green illumination of over sixty landmarks in mid-October 2020[38] or the ”Second Life Toys” campaign where old toys are gathered and their broken parts receive “transplants” from other toys, are noticeable but not necessarily informative. A lack of information or misinformation are listed among the reasons for the limited number of organ donations in numerous regions of the world.[39] Broadly available, specific and informative campaigns would not guarantee any increase in organ donations in Japan, but the lack thereof can be considered a factor hindering development in this area of medicine, especially in the context of the Wada incident’s influence on the attitude of the Japanese towards the procedure.
One of the problems surrounding organ procurement from brain-dead donors in Japan in the late 1990s was extensive press coverage, which was both caused by and at the same time fuelling a heated national debate. The limited number of transplants caused vivid media interest – the first transplant after passing the Organ Transplant Law in 1997 was reported in great detail by hundreds of journalists who had surrounded the hospital and started the coverage even before the family gave its consent to the operation.[40] While media interest has decreased over the past two decades, organ donations from brain-dead donors are still rare, and consequently, draw media attention, especially in the case of procurement from minors.[41] Media coverage raises awareness of the importance of organ donation, but unwanted attention directed towards bereaved families causes unnecessary pressure and forces the potential donor’s family to deal with yet another stressful issue.
Considerable media coverage has also been given to some influential critics of the concept of brain death and transplantation in general. The popular philosopher Takeshi Umehara (1990) publicly stated that brain dead patients cannot be considered truly dead since the idea of such death and transplantation in general are based on the Western dualistic perception of the body and soul, one which is incompatible with Japanese worldview. A slightly different stance was taken by the prolific writer Michi Nakajima (1985), working within the field of medical ethics and law, who accepts the necessity of performing transplants, but rejects the concept of brain death.[42] A broad overview of reasons for refraining from organ donation in general was given in the 2000 publication I don’t donate organs (Watashi wa zōki o teikyō shinai), in which popular writers and specialists discussed four aspects of transplantation: medical, philosophical, religious and journalistic, and in every case reached the conclusion that the procedure is problematic and inadvisable. Further research would be necessary to evaluate the volume’s actual role in shaping readers’ opinions, but positive online reviews supported by statements like “I cannot sign the donor card after reading this book” and “I realized [while reading] that maybe I didn’t care for my body [since I registered as donor]”[43] indicate that the publication did not remain without any influence on readers’ judgements.
In 21st century Japan, numerous factors intertwine and create a complex reality in which organ donations from deceased donors are slowly becoming accepted/acceptable. Attitudes towards death itself are visibly changing, and the impact of traditional taboos related to dead bodies is decreasing which is visible in the sharply growing number of body donations for anatomical training.[44] The concept of brain death, however, is still met with significant mistrust, preventing a considerable increase in organ donations.
According to scientific criteria, the medical understanding of death is identified with a dissociated process, not with a momentary phenomenon such as a one-time act of separating the soul from the body. In agreement with the medical findings, the death of individual cells, tissues and organs is a process that occurs over time, so the functions of some systems and organs may persist despite the death of other organs. Nevertheless, this process causes a progressive disintegration of the body as a functional whole which is why it leads to death.
Theocentric and empirical explanations for the end of human life differ from each other. There is still a debate as to whether brain death is the correct criterion for human death.[45] In the opinion of Maria-Keiko Yasuoka,[46] Yutaka Kato[47] and Nobuhiro Ooba,[48] the notion of brain death is not immune to criticism.
Some researchers from Japan have been investigating the causes for the social unacceptance of brain death as the overarching criterion for human death and according to Y. Kato and M.K. Yasuoka, cultural factors have a major impact on the medical understanding of death. For many Japanese people, the sole reason for consent to donate organs after their own death is associated with the recognition that permanent brain damage is an overriding criterion for the end of human existence. A widespread acceptance of this concept raises doubts because it is in contradiction with the assumptions of monistic philosophy, i.e., the location of the human spirit throughout the body, the tradition of gotai manzoku and respect for the integrity of the human body. In addition, for many Japanese people, the death of the brain does not mean the death of a person in a biological sense, and therefore it is not universally accepted that patients in an irreversible coma are dead.[49]
Worldwide changes in the definition and diagnosis of the end of human life were announced on the basis of a report delivered by the members of a Harvard University committee in 1968. Henry K. Beecher (Chairman), Raymond D. Adams, A. Clifford Barger, William J. Curran, Derek Denny-Brown, Joseph Murray, and Ralph Potter defined the state of irreversible coma as a new criterion for human death. The report reads:
“Our primary purpose is to define irreversible coma as a new criterion for death. There are two reasons why there is need for a definition: (1) Improvements in resuscitative and supportive measures have led to increased efforts to save those who are desperately injured. Sometimes these efforts have only partial success so that the result is an individual whose heart continues to beat but whose brain is irreversibly damaged. The burden is great on patients who suffer permanent loss of intellect, on their families, on the hospitals, and on those in need of hospital beds already occupied by these comatose patients. (2) Obsolete criteria for the definition of death can led to controversy in obtaining organs for transplantation.”[50]
In the course of the discussion on death, the commission recognized brain as the superior organ. Its permanent damage would lead to the loss of the organ integrating the whole body. The document issued by the committee members has become important for the development of medicine. On one hand, this information has introduced a new paradigm to thanatology. On the other, it has contributed to an increased organ supply in many countries around the world.[51] The decision made by the committee representatives led the classic definition of death (cardiopulmonary - respiratory) to give way to brain death, so the concept of the death of the body as a materially integrated whole became secondary to the cessation of brain stem activity, because its irreversibility means the loss of functions fundamental for human life.
Amendments to the definition of the end of life, which were first put into law in Japan in 1997, were met with resistance from society.[52] Japanese citizens did not accept this new definition of death because it did not take into account cultural aspects, respect for traditions and the beliefs of its citizens.[53] For this reason, brain-dead patients are not considered deceased because they have not completely lost integral bodily functions in a biological sense.[54]
To explain the criticism of this new definition of death, scientists from Japan, Great Britain and the United States have referred to the arguments of Alan Shewmon (an American neurologist at the University of California, Los Angeles), who has proven that there are signs of activity of certain parts of the brain in patients with brain death. The most important of them are:
Shewmon and other scientists have highlighted a number of integral body functions that are preserved in patients who are in a state of brain death, which is why they propose developing more accurate brain monitoring methods to be applied during resuscitation. In addition, Japanese doctors such as Tetsuo Kanno from the Fujita University of Health and his student Isao Morita have conducted innovative surgeries around the world. The surgery involves the implantation of a stimulator into the spinal cord to wake patients from a coma. The results of these operations are promising. Of 201 patients treated by this method, 109 patients responded positively on it and 7 of them regained consciousness.[60]
Innovative experiments involving stem cells and electrostimulation are the main directions taken by the development of medicine in Japan.[61] Scientists want to develop effective methods for waking coma patients as well as produce human organs from pluripotent stem cells in regenerative medicine facilities. The purpose of reproductive biology is to promote the development of innovative research on organ regeneration, which in the future might solve the problem of organ shortages not only in Japan, but also in other countries around the world.
The Organ Transplant Law of Japan was enacted in 1997. Its provisions were to increase the supply of organs in the country, but they proved to be too restrictive. Under these regulations, it was established that patients under the age 15 were not allowed to participate in organ transplants, and that society defined human death on the basis of the cardiopulmonary criterion, which is why the majority of Japanese residents did not accept organs from patients who were declared dead on the basis of brain death.[62]
The regulations introduced in 1997 did not lead to an increase in the number of organs collected but had a great influence on transplant tourism. Older residents of Japan who struggled with diabetic kidney failure have been going to the Philippines and China to buy organs, and for this reason the TTS – (Transplant Society) decided to issue the Istanbul Declaration in 2008 in order to urge individual countries to oppose organ trading, develop organ transplantation procedures and maintain safety procedures.[63] In 2010, WHO (World Health Organization) adopted new guidelines and amended international regulation.[64] The consequences of these decisions have had a major impact on the legislation in Japan. The new regulations were adopted on July 13, 2009, and by July 17, 2010 this law was already fully enforced there.[65] The amendment to the transplantation law introduced the following changes:
The aim for eliminating the lower age limit was to allow transplantations also among infants and children.[66]
Nevertheless, this topic still raises concerns among Japanese scientists. According to Masahiro Morioka, children diagnosed with brain death have a specific ontological status, that is, they have a natural right to death and no one can deprive them of this right, unless they have previously declared their desire to waive it. This concept is called the principle of wholeness and means that any person experiencing life or death should be equally protected from the expansion of biomedicine and other advanced forms of biotechnology.
According to the principle of wholeness, every person is a whole (psychophysical unity) being at every stage of life, so they should be inviolable.[67]
Masahiro Morioka, like Doyen Nguyen, defends the concept of a holistic human nature. According to this, human beings cannot be reduced to any particular characteristics — mental or organic —although self-awareness and cognitive function are the most distinctive features that distinguish humans from other animal species. Mental and organic properties, although different from each other, are interrelated and constitute a unity.[68] The opponents of this theory were Descartes and John Locke, who separated the abovementioned properties. On the basis of their philosophical views, John P. Lizza distinguished human death from the death of the human organism, explaining that with the irreversible loss of mental functions, the patient loses the status of a human and becomes only a living being or a biological artifact.[69] Viewing brain dead patients as humanoid beings is contrary to Masahiro Morioka’s views, for whom awareness is not the only condition for continuing life.
In Japan, the introduction of the family priority principle was to sanction the transfer of organs to the patient’s relatives, and the purpose of the legal regulation of brain death was to recognize an irreversible and permanent coma as the main criterion for human death.
Sanctioning brain death would not only align legal regulations in Japan with international standards but would increase the supply of organs because ex mortuo transplants offer the possibility of collecting and transplanting more biological material from one donor.[70] The introduction of the new transplant law was therefore intended to serve utilitarian purposes. Legislators hoped that the new regulations would alleviate the society’s reliance on the traditional views on death enough that they would accept the changes in defining the end of human life.[71]
The consequences of the adopted regulations were not as promising as had been initially hoped for. Information on this subject is presented in Table 1.
| Years | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 |
|---|---|---|---|---|---|---|---|---|---|
| Donors after brain death | 32 | 44 | 45 | 47 | 50 | 58 | 64 | 76 | 68 |
| Donors after cardiac arrest | 81 | 68 | 65 | 37 | 27 | 33 | 32 | 35 | 29 |
| Total score | 113 | 112 | 110 | 84 | 77 | 91 | 96 | 111 | 97 |
In the years 2010–2018, the introduction of changes to the provisions of medical law did not have a significant impact on increasing the supply of organs in Japan (Table 1). Despite the fact that there has been an increase in the number of organs retrieved from brain dead organ donors since 2013, this does not mean that society has recognized this condition as paramount. Despite the adoption of the transplantation law, Japan allows for the criterion of brain death only in justified circumstances, - i.e., when organ transplantation is to be carried out. Nevertheless, the majority of citizens still recognize cardiopulmonary criteria as the most important and decisive ones for the death of a person.[73]
For 12 years, the government in Japan has been looking for a suitable method to convince the public of this new definition of death in order to improve the rates of transplantology. It has been decided, for example, to change the content of the donor card. The second edition, issued since 2009, differs from the first one in that it allows consent to organ transplantation when the applicant accepts a) both neurological and circulatory criteria, or b) only one of them – the traditional assumption, i.e., the cardiac death (Fig. 1). The previous document separated the two criteria.[74]
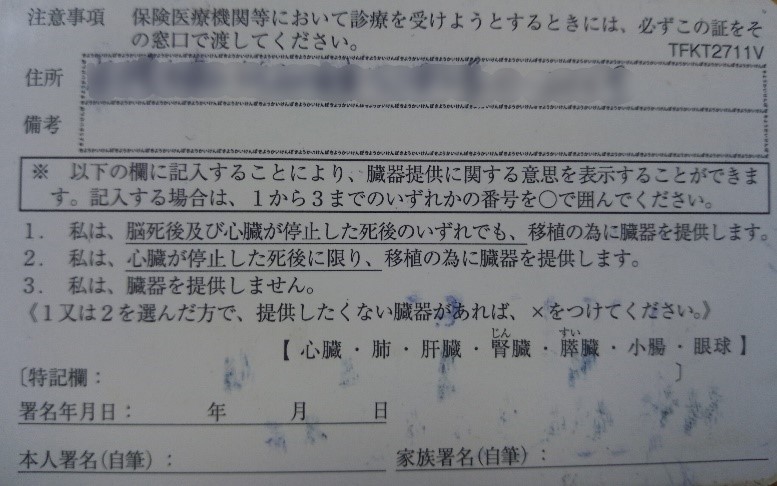
Fig. 1 Organ Donation Decision Card
By filling out the column below, you can state your will concerning organ donations. Please mark with a circle one option from 1 to 3:
(To those who chose 1 or 2: if there are any organs you do not wish to donate, mark them with an X.)
Heart, Lung, Liver, Kidney, Pancreas, Small intestine, Eye
Date
Signature of the card holder Signature of a family member
(Photo by Aleksandra Jaworowicz-Zimny)
Data from IRODaT confirm this information (Table 2). Over the years 2010–2018, the number of organs retrieved from living donors was much higher than those from deceased donors. These results lead to the conclusion that the Japanese support the idea of transplantation, but only in exceptional circumstances, mainly in the case of family diseases. In other words, they support it in cases such as when a relative is waiting for an organ transplant, e.g., a kidney (statistically, it is the organ most commonly retrieved in Japan). It is also worth noting that in 2017 IRODaT did not provide information on organs retrieved from living donors. Detailed information on this subject is provided in the 2018 Fact Book of Organ Transplantation in Japan. According to its statistics, the number and type of organs retrieved from living donors are the following: kidney – 1544, liver – 347, and lung – 10. It can be concluded that over the past 9 years, the inhabitants of Japan, if they consented, primarily opted for ex vivo transplants.
Table 2. The number and type of organs taken from living and deceased donors in Japan over the years: 2010–2018[75]
| Years |
|
|||||||||
| Kidney | Liver | Pancreas | Heart | Lung | ||||||
| d | l | d | l | d | l | d | l | d | l | |
| 2010 | 186 | 991 | 26 | 463 | 2 | 23 | 14 | |||
| 2011 | 211 | 0 | 41 | 0 | 35 | 31 | 37 | |||
| 2012 | 193 | 1412 | 41 | 382 | 27 | 28 | 33 | |||
| 2013 | 155 | 1431 | 39 | 369 | 33 | 38 | 41 | |||
| 2014 | ||||||||||
| 2015 | 167 | 0 | 45 | 0 | 35 | 44 | 45 | |||
| 2016 | 177 | 1471 | 57 | 381 | 38 | 52 | 50 | |||
| 2017 | 191 | 0 | 69 | 0 | 43 | 56 | 56 | |||
| 2018 | 182 | 1683 | 60 | 342 | 34 | 55 | 71 | |||
When comparing the IRODaT data for Japan to that of the South Korea, no such disparity is observed: a similar number of organs was obtained in south Korea from deceased and from the living donors in 2018. The total number of organs collected from deceased donors was 1502, and from living persons 1405.[76]
Akabayashi, Nakazawa and Ozeki-Hayashi hope that understanding why transplantology has been socially accepted by the inhabitants of South Korea creates the possibility of its application in Japan.[77] According to statistics from 2015 provided by KOSIS (Korean Statistical Information Service), Korean society is very diverse in terms of religion – 27.6% of the population of South Korea are Christians, 15.5% are Buddhists, and 56.1% are irreligious. In comparison, the percentage of non-religious people in Japan did not change between 1973 and 2018. According to the data published by NHK World Japan, almost 30% of the Japanese declare that they do not practice any religions,[78] therefore the religious beliefs of the Japanese have a limited influence on their views of organ transplantation and brain death, so it should not be considered that they are the main reason for not accepting transplantations ex mortuo in this country.
The attitude of South Korean citizens to transplantology is a very good comparison to Japan. In South Korea, neither religious pluralism nor the high percentage of non-religious people influences the acceptance rates for ex vivo and ex mortuo transplants. The inhabitants of Japan, who also declare a high diversity of worldview in statistical surveys, could in principle present similar views on transplantology as the inhabitants of South Korea, but they do not. Despite the fact that religions are a product of culture, they are not the only factor shaping the beliefs about death. The South Korean government officials have seen this, and in order to increase organ donation rates, they proposed specific changes by introducing: incentives programs, an organ procurement organization (OPO), donor registry and a potential donor referral system, which made it possible that the number of organ donations by brain-dead patients in South Korea reached about 10 per million people in 2013.[79]
Currently, government representatives in Japan are introducing a similar program, expecting similar results. Information on this will be explained in detail in part 5 of the article.
According to Akabayashi, Nakazawa and Ozeki-Hayashi, the changes initiated by the 1997 legislation and revised in 2009 had no effect on convincing the public to give their full consent to organ transplants from people who were declared dead due to brain death. The culturally shaped notion of human death continues to play an important role among Japanese citizens and, given the traditional convictions of the population, change should be based on the gradual introduction of reforms in the health and education sectors rather than on restrictive regulations. In line with this idea, the abovementioned researchers have proposed the following strategies:
The transplantation coordinator’s function is to organize, supervise and integrate the multidisciplinary work of transplantation teams. The coordinator’s tasks include identification and qualification of organ donors, care for the donor and the transplant recipient, monitoring multi-organ donations, as well as allocation, distribution and transplantation of organs. In addition, the transplantation coordinator is responsible for shaping the image of clinical transplantology within the broader society. An especially important part of their role is to talk to the deceased donor’s family to obtain consent for transplants. To develop these skills, coordinators need to acquire specialist knowledge in the field of clinical transplantology, immunology, intensive care, as well as in clinical psychology. In order to educate new hospital personnel and regional coordinators, additional training should be conducted for each hospital throughout the country. According to data from December 23, 2017, 93 transplantation coordinators were registered in Japan (33 employed by JOTN and 60 in prefectures).[80] In comparison, the Polish Poltransplant already employed 218 coordinators by 2015.[81] Additional education will allow medical staff to learn the correct methods at every stage of the transplant process, from identifying donors and legal requirements to talking to the family, as well as the organizational and logistical dimensions.
At the end of March 2017, there were 391 transplantation centers in Japan.[82] Many of these medical facilities did not have an efficient organ transplant systems in terms of legal provisions and organization. The lack of standardized guidelines in the protocol regarding the possibility of organ donation and transplantation inhibited the development of transplantation procedures throughout the country. Japanese medical experts such as Akira Akabayashi, Eisuke Nakazawa and Reina Ozeki-Hayashi drew attention to this fact and proposed that each hospital should have its own transplantation center. They also highlighted that the need for hospital and regional coordinators would increase with the number of facilities. These scientists believe that the provision of qualified medical personnel would make society familiar with the possibilities of transplantation.
Due to the decision of the Ministry of Education, Culture, Sport, Science and Technology (MEXT, Monka-shō), changes were made to the secondary school curriculum in Japan in 1989. The new provisions stated that the textbooks for teaching ethics and bioethics should contain information about brain death and organ transplantations. In 1994, seven out of nine textbooks’ manuals contained the updated guidelines.[83] As a result of these changes in the curriculum in the 1990s, people who are now in their 20s and 30s have both more knowledge and awareness of organ donation than older Japanese residents.
The government’s policy to promote transplantation has not stopped with the above decision, as it was agreed that from 2017 onwards, all ethics and bioethics textbooks for secondary schools should include information on brain death and transplantation. The Ministry has estimated that by 2050 not only younger but also older Japanese citizens will consent to retrieving organs from the deceased.
The government project was aimed at high school students, but it is worth considering whether, given the current legal possibilities of organ harvesting from children and infants, the subject of transplantation should not be introduced into the ethics and bioethics curriculum for primary school children.
The JOTN organization introduced the possibility of the electronic registration of donors in 2017.[84]
The Japanese donor card allows potential donors to choose death criteria as well as specify organs for donation. Nevertheless, the information on this subject is in Japanese, and it constitutes a significant difficulty for the 2 million foreign residents who do not speak this language. Given the language obstacles, a document such as a donor card should be translated into English.
Akabayashi, Nakazawa and Ozeki-Hayashi have suggested changes to the system of organ procurement and transplantation based on the model adopted by the USA. “The Organ Procurement Organization” (OPO) is a non-profit association in the United States responsible for the evaluation and retrieving organs from deceased donors. There are 58 such organizations in the United States, each coordinating the implementation of transplantation targets in its region. In addition, each of them is a member of “The Organ Procurement and Transplantation Network”,[85] a federally authorized network set up and supervised by “The United Network for Organ Sharing” (UNOS).[86] Qualified medical workers employed by OPOs have direct contact with the hospital and the family of the deceased donor and try to persuade their relatives to agree to the removal of organs. Once OPO workers receive family consent, they work with UNOS to oversee transplant surgery.
The Japanese organization JOTN combines the functions of these two entities (OPOs and UNOS).[87] However, hospitals in Japan that have intensive care units, operating rooms and ambulance services are not legally obliged to report patients who have died of brain death, especially if they are not eligible as potential donors. On the other hand, such an obligation exists in the United States, so it is not possible for potential donors to be omitted.
The failed first heart transplant, the “Wada incident” of 1968, influenced the public perception of transplantation in Japan. For over 50 years, the Japanese government has been trying to change the public’s attitude towards organ transplants by introducing changes to the legal regulations. Nevertheless, the views of older Japanese citizens remain largely unshifted.
This is mainly due to cultural considerations: the gotai manzoku tradition and respect for the integrity of the human body.
Given this fact, the most difficult task is to convince the public to consent to organ retrieval from people who have been declared dead as a result of brain death, and for this reason the government has decided that stopping at the mere revision of the law is not an effective solution to the problem.
Currently, discussions are underway in Japan to implement an appropriate strategy. Some Japanese scientists such as Akira Akabayashi, Eisuke Nakazawa and Reina Ozeki-Hayashi have proposed changes in the health and education sectors. Particularly noteworthy has been the introduction of reforms to the ethics and bioethics curriculum. This idea has gradually changed the attitude of the younger generation towards transplantology since 1994. Researchers concluded that the awareness of teenagers has increased with the spread of knowledge. Young people accept the criterion of brain death faster, which is why they declare consent to organ removal more often than older people. According to the above-mentioned scientists, this method should be continued.
In addition, researchers are looking for similar results by increasing the number of transplantation coordinators, developing transplant centers, as well as improving the registration process of organ donors and recipients.
All of these ideas should increase the number of organs collected, so that in the future every Japanese citizen will have the opportunity to use this method of treatment in their own country.
Although the changes proposed by these Japanese scientists serve to promote the idea of transplantology, they may not convince the whole of society to accept the concept of brain death. It is therefore important to respect both the cultural and religious beliefs of the people of Japan. How we understand the phenomenon of death often depends on a person’s philosophical and religious views and, as Masahiro Morioka wrote, „these different views on death are not irrational”.[88]
According to monistic philosophy, it is assumed in Japan that the essence of humanity is not self-awareness and rationality. Its essence exists in both the mind and the human body. The result of the union of soma and psyche is the personification of the human body. Carnality acquires the characteristics of a person, so it ceases to be only a mechanism that serves the psyche. Thus, respect for the person becomes inseparable from respect for his living body.
In addition, not only Japanese residents express doubts when choosing brain death as the criterion of human death. Problems with its acceptance also occur in Germany and Denmark, where 20% to 40% of society declares their concerns.[89] This is confirmed by the fact that the phenomenon of death is not only a medical issue, but also a cultural construct. Many people expect the right to choose a death criterion according to their beliefs.
Justyna Czekajewska is responsible for the concept, methodology and supervision of the article. Justyna Czekajewska and Aleksandra Jaworowicz-Zimny are responsible for collecting and reviewing the literature. Justyna Czekajewska and Aleksandra Jaworowicz-Zimny are responsible for writing and critically reviewing the article. All authors read and approved the final manuscript.